Send Claims
View claims waiting to be sent, a history of sent claims, validate and send claims, and more.
In the Manage Module, click Send Claims.
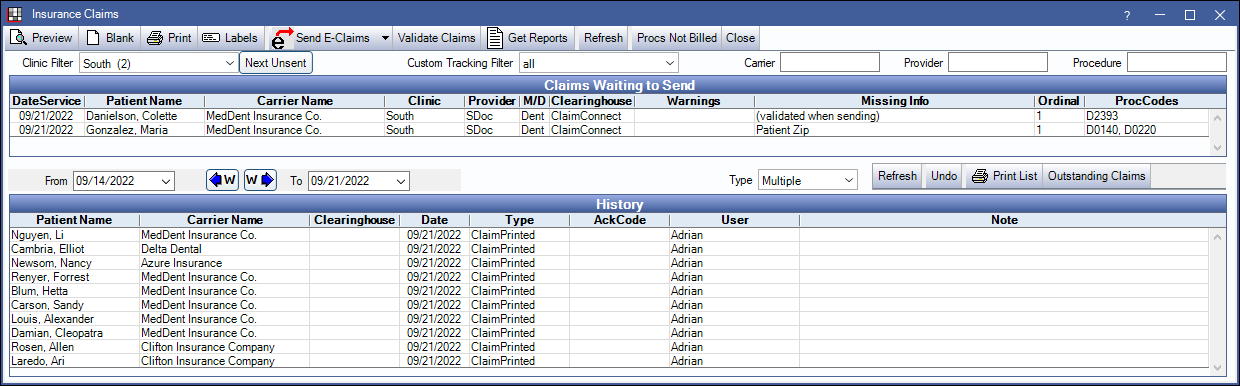
Insurance claims can be sent, printed, and managed on the Insurance Claims window.
- Print or send claims as part of a batch..
- View a history of sent claims, printed claims, and reports.
- View and process ERAs received from a clearinghouse.
- Create batch claims for unbilled procedures. See Procedures Not Billed to Insurance Report.
This window is non-modal so users can open other windows while sending or validating claims.
Toolbar
- Preview: View the selected claim before sending or printing. Users can also double-click a claim in the grid to preview.
- Blank: Print a blank version of the default claim form.
- Print: To print specific claims, select them, then click Print. To print all claims marked as Paper, do not select any claims, then click Print.
- Paper claims are defaulted when the preference for Send Electronically is set to Don't usually send electronically in the Insurance Plan.
- Printing a claim automatically changes its status to sent.
- Labels: Print individual labels for selected insurance carriers.
- Send E-Claims: All claims will be validated before sending to ensure no information is missing.
- To send all claims as a single batch to the clearinghouse listed in the Clearinghouse column, click Send E-Claims or click the dropdown to select the clearinghouse. A confirmation message will show. Click Yes to proceed.
- Claims with Paper as the clearinghouse will be ignored.
- For e-claim troubleshooting, see E-Claims Complexities.
- Validate Claims: Validate selected e-claims for missing information prior to sending.
- Royal dental Software always validates e-claims when sending. If a claim has missing information, no claims in the batch will send and Missing Info will list in the last column. If a claim has already been sent, a warning will show and the claim will not be resent.
- To validate claims when the Insurance Claims window loads (before sending), enable the Preference Claims Send window validate on load. This may be useful for smaller offices.
- Get Reports: Manually retrieve reports from a clearinghouse. See Reports below.
- Refresh: Update the Claims Waiting to Send grid.
- Procs Not Billed: Open the Procedures Not Billed to Insurance Report and optionally create batch claims for unbilled procedures.
- Close: Close the window.
Claims Waiting to Send
The top half of the window lists claims that have a status of Waiting to Send. Click a column header to sort.
Filter options:
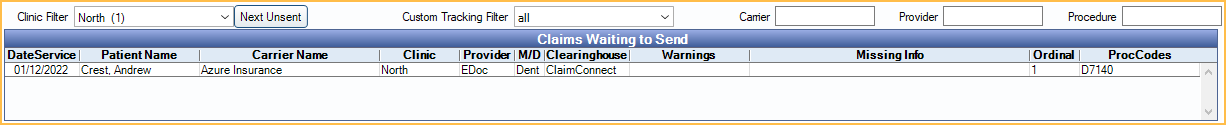
- Clinic Filter: Only visible when Clinics is turned on. Filter claims by clinic to easily send each clinic's claims to a specific clearinghouse. The logged-on user must have access to a clinic to view or send claims for that clinic.
- Next Unsent: Automatically select the next clinic with unsent claims.
- Custom Tracking Filter: List claims by recorded claim tracking status. Custom tracking data is entered on the Edit Claim - Status History Tab.
Columns:
- DateService: Date of service on the claims. Dates showing 01/01/0001 indicate a preauthorization.
- Patient Name: The patient that is attached to the claim.
- Carrier Name: The insurance plan attached to the patient.
- Clinic: If using clinics, the clinic the claim is associated with.
- Provider: The treating provider on the claim.
- M/D: Indicates whether the claim is Medical (Med) or Dental (Dent).
- Clearinghouse: Determined by the insurance plan's setting for Don't usually send electronically (Insurance Plan). If checked, paper will list. If unchecked, the default clearinghouse will list.
- Warnings: Indicates when a user attempts to send a deleted or already sent claim.
- Missing Info: Indicates the claims validation status. If validated when sending, the claim has not been validated for missing information yet. If missing information is listed, it must be completed before resending. Right click on the claim to Go To Account. If the column is blank, the claim has been successfully validated with no missing information found.
- Ordinal: Order of insurance plan set in Patient Information section of Edit Insurance Plan window (e.g., 1, 2, etc). Indicates if plan is primary, secondary, etc.
- ProcCodes: Procedures attached to the claim.
Claim History
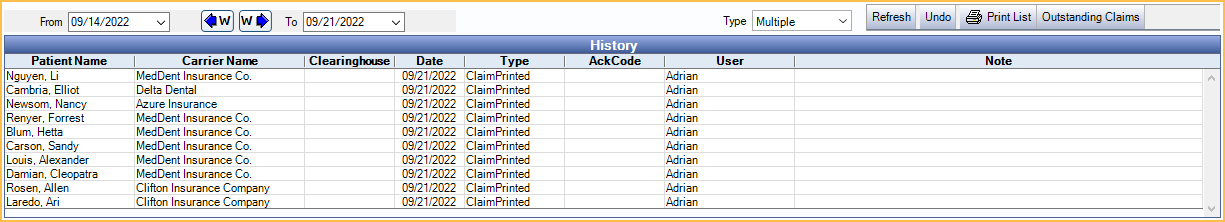
The lower History grid lists all claims sent or printed from this window and received reports (e.g., ERAs, acknowledgment reports). Double-click an item to view more information. Right click an item to Go To Account. The list of claims and reports can be filtered by date or type.
Filter Options:
- Date From / To: Only show claims and reports in a date range.
- Manually enter the dates.
- Click the down arrow to select dates from a calendar then click the up arrow to collapse the calendar.
- Click the W buttons to jump back or forward one week.
- Type: Only show certain types of claims or reports. Single click an option, or to select multiple. If no options are selected, then all types will show.
- ClaimSent
- ClaimPrinted
- Claim_Ren: Renaissance claims.
- StatusNotify_277: A health care claim 277 acknowledgment that notifies of claim status. See Acknowledgment Reports below.
- TextReport: Any report that is not a 997, 999, 277, or ERA_835. See Text Reports below.
- ERA_835: A electronic EOB, also known as electronic remittance advice or ERA. The AckCode indicates the ERA status. If blank, some or all claims on the ERA are not received. If Received, all claims have been received, but payment must be finalized. Double-click an ERA to process it.
- Ack Interchange
- Refresh: Refresh the list.
- Undo: If there was a problem with sending, highlight the claims and click Undo. The claims will move back to the Claims Waiting to Send grid. Claims will still be listed in the Claim History grid for historical record.
- Print List: Print the current contents of the History grid.
- Outstanding Claims: Open the Outstanding Insurance Claims Report.
Columns:
- Patient Name: The patient that is attached to the claim.
- Carrier Name: The insurance plan attached to the patient.
- Clearinghouse: The clearinghouse that the claim was sent to, where applicable.
- Type: Displays the type of claim or report. See Type, above.
- AckCode: The status on a Claim Ack 277. This column will show A or R (accepted/rejected).
- User: The logged-on user that sent the claim, where applicable.
- Note: Double-click the item to enter a note in this column.
Claim Details
To view details about a sent claim, double-click it.
If there is ever any need to troubleshoot a sent claim, the full text of the batch is saved here. Most of the text, as well as the fields below, are meaningful only to technical support.
Attachments Sent: Indicates if attachments were sent.
Note: Add a note that will display on the Insurance Claims window.
Acknowledgment: If the transaction has been acknowledged by the clearinghouse, then that information, including the full Message Text and Date/Time, will show at the right.
Reports
In order for a report to list in the History grid, it must first be downloaded to the Clearinghouse Report Path.
- To set up automatic download, see Clearinghouses. Only certain clearinghouses allow automatic download.
- To manually download, click Get Reports or manually save the report file to the correct report path.
Reports can only be retrieved once per minute. If a user attempts to retrieve reports more than once in a minute, they will get an error. As reports are retrieved a progress bar will appear. Errors will be recorded in the Error Log. Users can pause or cancel the progress at any time.
Acknowledgment Reports: There are 4 types of acknowledgment report formats; 997, 999, 277, and 835. They are listed in the order in which they are received from the clearinghouse. Clearinghouses are not obligated to provide these acknowledgment reports and may choose to return some or all reports for some batches and not others.
- 997 & 999: Royal dental Software has supported format 997 (functional acknowledgment) for years. Support for format 999 (implementation acknowledgment) was added in Version 12.3. The 997 and 999 are simpler formats that only provide information regarding the status of a batch based purely on formatting and data requirements. When a 997 or 999 is received by Royal dental Software, the AckCode column in the History grid for the corresponding claims are set to A for accepted or R for rejected. To view the acknowledgment message text, double-click on the sent claim.
- 277: Shows in the History grid with a Type of StatusNotify_277. This report provides more detailed status information about the sent batch than a 997 or 999 format. Support for the 277 format was added in Version 12.3.
- 835: Also known as the electronic remittance advice or ERA. The 835 report shows in the History grid with a Type of ERA_835.
Text Reports: Reports usually come back from the clearinghouse as files placed in the report path specified in the Edit Clearinghouse window. They are then automatically imported by Royal dental Software and stored in the database. The original text file is deleted. Older versions of Royal dental Software did not store the report in the database, but instead moved the file to an archive folder. Because of the new way that reports are handled, it is no longer important to always run e-claims from the same workstation. However, if an office uses Tesia, then TesiaLink should only be running on one computer at a time. Also, there is no need to manually archive reports. Reports that have been imported will show as rows in the lower history grid. Double-click on the row to view or print. Use the Note field to make comments about each report that will be useful.
Some clearinghouses use a web-based follow-up system rather than sending back text reports.


