Fee Schedule Logic
See Procedure Codes.
The Fee Schedule used for procedure fee estimates is determined using the logic below.
Insurance
PPO Plan Types
Fee billed is based on the fee schedule (assigned in Edit Provider) of the the patient's primary provider. The fee schedule of the treating provider is not considered.
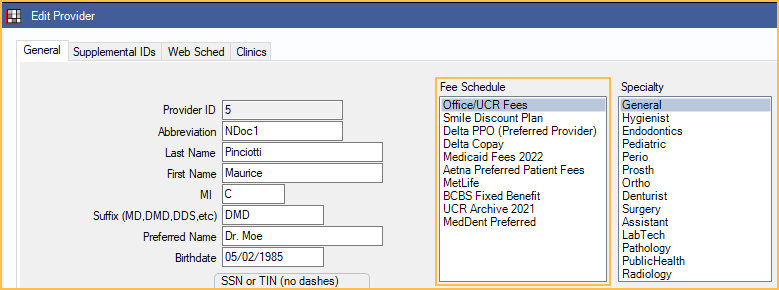
The fee schedule assigned in Edit Insurance Plan is used for write-off calculations. It does not affect the billed fee.
When using PPO insurance, if the preference, Use UCR fee for billed fee even if PPO fee is higher, is enabled, the provider fee will be used even if the PPO fee is higher. Disable this setting to always bill the higher fee.
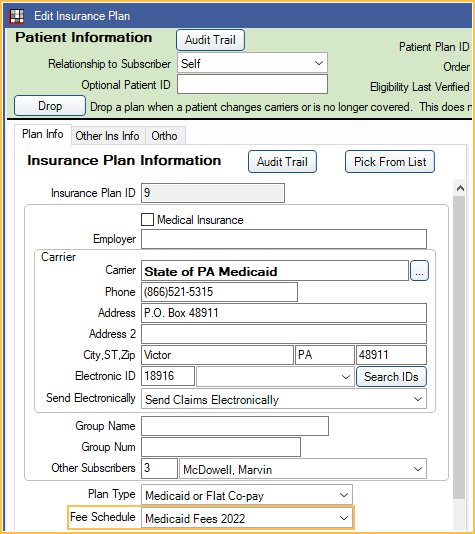
Category Percentage and Medicaid/Flat Co-pay Plan Types
The fee billed will be based on the Fee schedule assigned in Edit Insurance Plan window. If the patient has multiple insurance plans, the fee schedule of the first insurance plan listed in the Family module is used (e.g. order = 1 on the Insurance Plan).
If no fee schedule is assigned to the insurance plan, the fee will be billed in the following order:
Priority 1: Fee schedule assigned in Edit Patient Information (rarely used).

Priority 2: Fee schedule of the provider assigned to the procedure, if any (Assign to Prov on the Procedure Code).
Priority 3: Fee schedule of the provider assigned to the procedure's appointment or to any appointment scheduled today.
Priority 4: Fee schedule of the patient's primary provider.
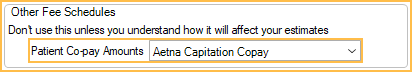
Capitation Plan TypesCapitation insurance does not normally bill any fee to the patient account. If the patient has a capitation insurance plan, using the Capitation Plan Type with a copay, the fee billed with be based on the copay fee schedule assigned in the Edit Insurance Plan window. If there is no copay for a procedure, the fee billed will be $0.
If the insurance plan is mixed capitation (HMO / DMO Insurance Plan with Copays and Supplemental Payments), the same logic applies as for PPO Plan Types as described above since these plans will use the PPO Percentage plan type.
No Insurance
If a patient does not have insurance, fees are billed in the following priority:
Otherwise, for patients without insurance, the fee schedule of the provider who has priority is used.
- Priority 1: Fee schedule assigned in Edit Patient Information (rarely used).
- Priority 2: Fee schedule of the provider assigned to the procedure, if any (Assign to Prov on the Procedure Code).
- Priority 3: Fee schedule of the provider assigned to the procedure's appointment or to any appointment scheduled today.
- Priority 4: Fee schedule of the patient's primary provider.
Also see: Discount Plans.
Medical
If the patient has medical insurance, the fee schedule of the first medical insurance plan listed in the Family module is used.
If a Procedure Code is a dental code cross-coded to a medical code, then the preference, Use medical fee for new procedures, determines the fee. If checked, the fee of the medical code is used; if unchecked the fee of the dental code is used.
Overrides
After the fee schedule is determined, then any Provider and/or Clinic-Specific Overrides are applied to that fee schedule.
For example, if the default fee for a procedure in the prioritized fee schedule is $110, but there is an override in that fee schedule for the treating provider of $125, the fee billed will be $125.
Setting up overrides is helpful in the case of specialist or clinic specific fees and should be done in lieu of setting up individual fee schedules for clinics or providers.
Copay Fee Schedule Tips
How a copay fee schedule should be created depends on the information sent by insurance.
- If the insurance fee schedule is the total amount you are allowed to collect (including patient copay amounts):
- Create the Patient Co-pay Amounts fee schedule.
- Create the insurance fee schedule using the amounts provided by the carrier.
- If the insurance fee schedule is the amount insurance is paying you (and patient copay is not included in the amount):
- Create the Patient Co-pay Amounts fee schedule.
- Create the insurance fee schedule by taking the insurance amount and adding the copay amount.
(e.g. if the insurance will pay $100, and the patient copay is $50, the fee schedule amount should show $150)